In a bushel basket, one bad apple spoils the bunch. In the brain, one bad protein can do the same. A misfolded protein can coax its neighbor into the same mangled shape; that protein does the same to its neighbor. In a slow-motion chain-reaction, a section of the brain gets clogged with infectious, misfolded proteins known as prions.
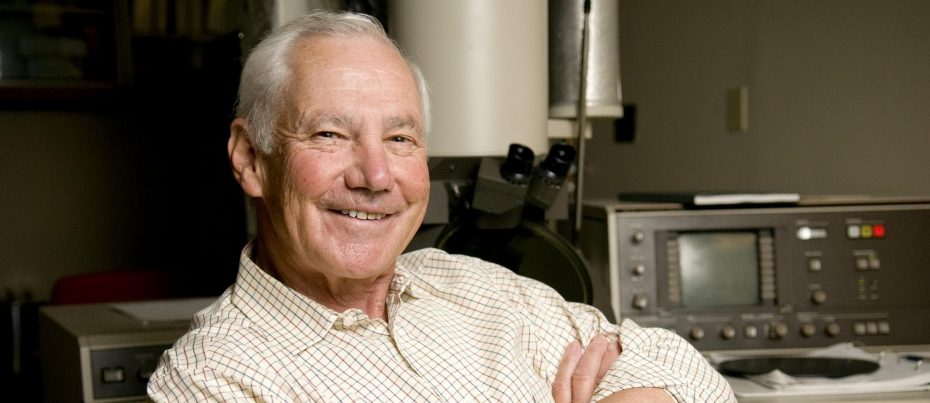
In the 1980s, biochemist/neurologist Stanley Prusiner discovered that diseases including Creutzfeldt-Jakob disease (CJD), scrapie, and mad cow disease were caused not by infectious viruses or bacteria, but by prions that overtook the brain like falling dominoes. For his discovery, Prusiner won the 1997 Nobel Prize in Physiology or Medicine and a 2010 National Medal of Science.
Today, Prusiner is still studying prions, but he’s set his sights on a different disease: Alzheimer’s. For decades, Prusiner has been convinced that Alzheimer’s disease is a prion disease—he proposed the idea in a 1984 New England Journal of Medicine article. Now, he’s gathering concrete data to convince the rest of the scientific community.

“All this other stuff that Alzheimer’s researchers are focused on is secondary—inflammation and microglia and blood flow—the list goes on and on,” says Prusiner. “All you really need to do is stop making prions.”
Of course, as with all science, that’s easier said than done.
Infectious Amyloid
In the brains of people with Alzheimer’s disease, pathologists see two proteins—amyloid-beta (Aβ) and tau—clumped into striking plaques and tangles. It’s well-accepted that the versions of Aβ and tau protein that form amyloid plaques and neurofibrillary tangles are misfolded. However, the idea that Aβ and tau are prion proteins has been less mainstream. For years, researchers have focused on lowering overall levels of Aβ to treat Alzheimer’s, but clinical trials have repeatedly failed.
“These drugs haven’t worked because they’re not specific enough,” Prusiner argues. “They’re not specific to the prion form of amyloid-beta.”
The challenge with studying prions is that in many experiments, it’s hard to tell the difference between the infectious prion form of a protein and the normal, healthy form. Each molecule contains the same amino acids—the basic building blocks of a protein—in the same order. To differentiate the proteins, one must study their structure. Measuring the amount of a prion in a patient’s brain has been especially tricky. In previous studies, Prusiner’s team injected brain extracts from Alzheimer’s disease patients into mice and tracked—over relatively long periods of time—whether the mice developed symptoms of the disease. But the approach was far from quantitative.
In a study published this spring in Science Translational Medicine, Prusiner and his colleagues came up with a new technique to solve this long-standing challenge. They engineered cells to fluoresce when the prion form of Aβ formed aggregates. Counting the fluorescent clumps of protein lets the scientists quantify the levels of Aβ prions. A similar approach had already been developed by another group of scientists to measure the prion form of tau.
Prusiner’s team used the approach to measure levels of Aβ and tau prions in postmortem brain tissue from 75 Alzheimer’s patients, ten healthy controls, and 21 patients with other neurodegenerative diseases. In Alzheimer’s disease brains, both Aβ and tau prions were detected, while in brain samples from people with frontotemporal lobar degeneration, only tau prions were present.
Although overall levels of tau increase with age in Alzheimer’s, the researchers found that levels of the tau prion actually decreased. Patients who died of Alzheimer’s at age 40 had, on average, 32 times more tau prions than patients who died at 90. Similarly, Alzheimer’s patients over age 80 had the lowest levels of Aβ prions.
It’s not immediately clear why tau prion levels are linked to longevity—do patients with fewer tau prions live longer? Or do levels decrease as a patient ages? But the results, says Prusiner, underscore how vital it is to look at prion levels, rather than overall protein levels, when it comes to Aβ and tau in Alzheimer’s. And the new test to measure Aβ prions can be immediately useful in better postmortem diagnosis of Alzheimer’s for research purposes.
“I’m very focused on developing therapies; that’s where I’m spending a huge amount of time right now,” says Prusiner. “To do that, we also need better detection for prions.”